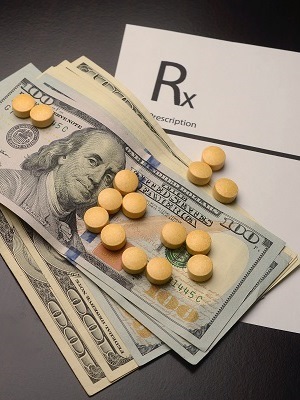
Rising drug prices in the United States will lead payers and
pharmaceutical benefit managers (PBMs) to increase the number of drugs
ineligible for reimbursement, subsequently challenging drug developers to step
up and provide more evidence that their products are clinically superior and
cost effective, a new report finds.
In fact, payers are responding to rising drug costs with more restrictive formulary management policies while PBMs are expected to expand their exclusion lists, concludes the report, Expected Growth in PBM Exclusion Lists Poses a Challenge to Drug Developers, from the Tufts Center for the Study of Drug Development (CSDD) in Boston.
These exclusion lists, which are meant to reflect clinical and cost effectiveness, contain the drugs that are ineligible for reimbursement, along with covered recommended alternatives in the same therapeutic class. Excluded drugs are those that purportedly offer no additional benefit over alternative treatments in the same therapeutic class.
Regarding formulary management, Joshua P. Cohen, research associate professor at the CSDD, said he expects that PBMs and payers will increase their use of more traditional approaches, including tiered formularies, prior authorization, step therapy, and off- and on-label indication restrictions — actions that in turn will challenge the biopharmaceutical industry to provide more evidence-based assessments of their products’ values.
And as more clinical and cost-effectiveness evidence is developed and used, he said he thinks that exclusion lists will likely expand, thereby increasing the role pharmacists play in facilitating formulary management.
“The pharmacies have always played an important role as enforcer, if you will, of formulary management tools implemented by PBMs, whether prior authorization rules or quantity limits or any number of traditional methods," Cohen told American Pharmacy News. "In the case of exclusions, they will be forced to use hard edits in some cases, facilitating changes of certain prescriptions from excluded to recommended products."
At the same time, Cohen said he doesn’t think this will necessarily be detrimental to patients, as choosing a more cost-effective medication is often the better choice.
“However, there is no average patient," he said. "And clinical and cost-effectiveness data is based on averages. Certain patients who don't fit the profile of ‘typical’ may be adversely impacted by the expansion of exclusion lists.”
But these expanded exclusion lists will impact a relatively small number of patients, he added.
“Perhaps as few as one million covered lives enrolled in Express Scripts or CVS Caremark," Cohen said. "Nevertheless, one million patients will see fewer choices of medications in certain classes and may be denied coverage if they wish to be prescribed the excluded products."
The report, Expected Growth in PBM Exclusion Lists Poses a Challenge to Drug Developers, is available here.








 Alerts Sign-up
Alerts Sign-up